Lead Exposure and its Impact on Your Health
Lead Exposure and its Impact on Your Health
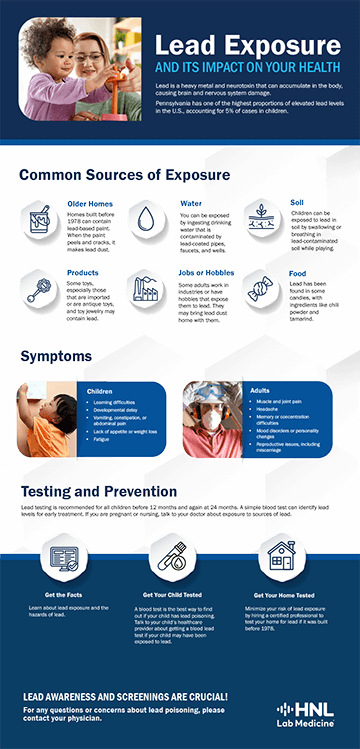
Lead Poisoning Prevention Week is the perfect time to learn more about lead and its health effects. Lead is a heavy metal and neurotoxin that can accumulate in the body, causing negative health consequences of the brain and central nervous system that may be permanent. Unfortunately, Pennsylvania has one of the highest proportions of elevated lead levels in the United States, accounting for 5% of total cases in children ¹. Because children’s bodies absorb and accumulate lead quickly, symptoms may develop when the blood lead reference value is as little as 3.5 micrograms per deciliter (µg/dL) ².
The over-accumulation of lead in the body, also known as lead poisoning, can result in irreversible intellectual disability, behavioral effects, and neurological effects including coma and death. According to the World Health Organization (WHO), 30% of the world’s idiopathic intellectual disability is caused by lead ³. In children, the overaccumulation of lead causes injury to brain and nervous system development.
Although lead testing is not mandatory in Pennsylvania, it is recommended for all children to be screened before 12 months, and again at 24 months. A simple blood test can identify levels of lead in the body, allowing patients to begin treatment as soon as possible.
Sources of Lead Exposure in Pennsylvania
Lead can be inhaled during manufacturing procedures that burn lead, like the smelting of lead batteries, processing recycling, and stripping lead-based paint. It can also be ingested through lead-contaminated dust or soil, water from leaded pipes, or food from lead-glazed containers.
In Pennsylvania, due to the number of older homes containing lead-based paint, the consumption of lead-based paint chips or inhalation of dust is one of the leading causes of lead poisoning, particularly in children. The use of lead-based paint was common in homes built before 1978. Older homes may also be at risk of lead-coated pipes, which can contaminate water sources.
Although lead-based paint was banned in the United States in 1978, it is still used by many countries. Only 45% of countries have lead-based paint control policies ³. Lead-based paint has been found on children’s toys. Antique toys and collectibles, even those made in the U.S., are potential sources of lead exposure.
Battery manufacturing and recycling plants employ and support many families throughout Pennsylvania. Employees must be regularly monitored through medical surveillance and blood testing to ensure the levels of lead in their blood are within allowable limits. The standard for industrial exposure and allowable levels are currently set at 40 µg/dL, although that level could still be too high for many workers, including those with health conditions, non-occupational lead exposure, accumulated exposure, or those with abnormal absorption rates ⁴.
In Pennsylvania, lead exposure can result from water sources using lead-coated pipes, faucets, and wells. Although the use of lead in the repair or construction of pipes and other plumbing fixtures was banned in 1991, older plumbing might still contain high levels of lead. Older institutional buildings such as those used by daycares and schools might be particularly at risk. While schools are not mandated to test their water sources for lead, a 2018 amendment to the Public School Code encouraged schools to do so. Since then, nearly 800 sources were tested against Environmental Protection Agency (EPA) actionable levels of 15 parts per billion (ppb). Some sources, which have since been disconnected or put out of service, showed lead exposure levels of 1350 ppb- 90x higher than actionable levels defined by the EPA⁵.
Other Sources of Lead Exposure
There are many consumer products which may contain lead, like plastics, jewelry, and toys. According to the Center for Disease Control and Prevention (CDC), because the use of lead in plastics creates a more flexible and heat-resistant product, it has not been banned⁶. When plastic is exposed to sunlight, detergents, or other products that break down its chemical bonds, lead dust can form.
Costume, toy, and vending machine jewelry has been found to contain high levels of lead. Because lead is not absorbed through the skin, the jewelry is safe to wear. However, children may be exposed to lead if the jewelry is put in the mouth or swallowed. Other items, such as antique dishware, silverware, and jewelry, may also be a source of exposure ⁶.
Certain food sources might contribute to lead exposure, particularly some types of candy, alternative medicines, and spices. An analysis of 50 spices from 41 countries was conducted between 2008 and 2017 to determine the number of spices containing lead over food actionable levels of 2 ppb. The analysis discovered the presence of lead in over 50% of the samples. In some spice samples, like Georgian saffron, lead was present in 100% of the samples. Georgian saffron had lead concentrations of up to 48,000 ppm. Other spices with a high concentration or occurrence of lead were curry, chili powder, masala, turmeric, and paprika ⁷. Candies and herbal remedies made from spices with high concentrations of lead will have high concentrations as well.
Symptoms of Lead Poisoning
Symptoms of lead poisoning in adults can include:
- muscle and joint pain
- headache
- memory or concentration difficulties
- mood disorders or personality changes
- reproductive issues including miscarriage
Symptoms of lead poisoning in children can include:
- learning difficulties
- developmental delay
- hearing loss
- vomiting, constipation, or abdominal pain
- lack of appetite or weight loss
- fatigue
Newborns exposed to lead might also be born prematurely, have a lower birth weight, and experience slowed growth ⁸.
Testing and Treatment
There are two primary testing methods for lead. A capillary sample can be tested using a finger or heel prick. This type of sampling can easily become contaminated by lead residue on the skin. Because of the possibility of contamination, a second capillary sample is needed to confirm positive results.
A venous sample, or blood draw, provides the most accurate blood lead levels because it is less likely than capillary sampling to be contaminated by lead on the skin. This type of sampling uses blood directly from the patient’s vein.
When elevated levels are detected, treatment can begin. Some treatment is simply preventative, which removes lead from the environment and prevents recurrent exposure. Replacing lead-coated pipes, resealing lead-based paint, or otherwise removing the sources of exposure can be enough to lessen elevated blood results, particularly in low levels. For adults and children with symptoms of lead poisoning or high blood lead values, the most common type of medical treatment is chelation therapy. In chelation therapy, medication is used to bind to lead particles, which can then be excreted from the body in urine. For severe cases, or patients who are unable to undergo conventional chelation therapy, EDTA chelation therapy is used. This type of chelation therapy uses a chemical called calcium disodium ethylenediaminetetraacetic acid (EDTA) to bind to lead and must be given as an injection ⁸.
In Conclusion
In Pennsylvania, children and adults have greater exposure to lead than other places, causing elevated blood lead levels and lead poisoning. In addition to common exposures through consumer products, food, and plastic, Pennsylvanians are exposed to unique sources of lead. The occupancy of older homes containing lead-based paint and lead-coated pipes, and employment in battery manufacturing and recycling processing can result in greater than average lead exposure.
Discuss any symptoms of lead poisoning with a physician. Testing for lead is easy and affordable, and in most cases is covered by programs such as Medicaid and Medicare. Medicaid requires and covers lead testing for children at 12 months and again at 24 months.
Lead Poisoning Prevention Week raises awareness of the common risk factors and exposures of lead poisoning. Be aware of products that may contain lead and sources of exposure in and around the home. Know how to recognize the symptoms of lead poisoning. Regular screening can catch lead poisoning in the early stages. Early chelation or preventative treatment can prevent permanent damage from lead poisoning. While the awareness campaign lasts one week, the recognition, prevention, and screening of lead poisoning should last all year.
References
¹ Hauptman, M., Niles, J. K., Gudin, J., & Kaufman, H. W. (2021). Individual- and community-level factors associated with detectable and elevated blood lead levels in US children. JAMA Pediatrics, 175(12), 1252. https://doi.org/10.1001/jamapediatrics.2021.3518
² Center for Disease Control and Prevention. (2022, December 02). Blood lead reference value. U.S. Department of Health and Human Services. https://www.cdc.gov/nceh/lead/data/blood-lead-reference-value.htm
³ World Health Organization. (2023, August 11). Lead poisoning. https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health
⁴ Occupational Health and Safety Administration. (2019, May 14). 1910.1025 App B - Employee standard summary. U.S. Department of Labor. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1025AppB
⁵ Pennsylvania Department of Education. (2023, August). Information for Schools: Lead in Drinking Water. Commonwealth of Pennsylvania. https://www.education.pa.gov/Schools/safeschools/resources/Pages/Lead-in-Drinking-Water.aspx
⁶ Center for Disease Control and Prevention. (2023, June 23). Lead in consumer products. U.S. Department of Health and Human Services. https://www.cdc.gov/nceh/lead/prevention/sources/consumer-products.htm
⁷ Hore, P., Alex-Oni, K., Sedlar, S., & Nagin, D. (2019). A spoonful of lead: A 10-year look at spices as a potential source of lead exposure. Journal of Public Health Management and Practice, 25(1). https://doi.org/10.1097/phh.0000000000000876
⁸ Mayo Clinic. (2022, January 21). Lead poisoning. https://www.mayoclinic.org/diseases-conditions/lead-poisoning/diagnosis-treatment/drc-20354723